Dental implant treatment has long moved beyond a purely surgical procedure and is increasingly regarded as a complex biomechanical task. Professor Alexander von Breuer emphasises that the key factor in long-term implant success is not the act of placement itself, but the ability of the construction to withstand functional load over the years. At DentalClinic24, assessment of implant overload risk is performed at the treatment planning stage and is considered an essential component of clinical analysis.
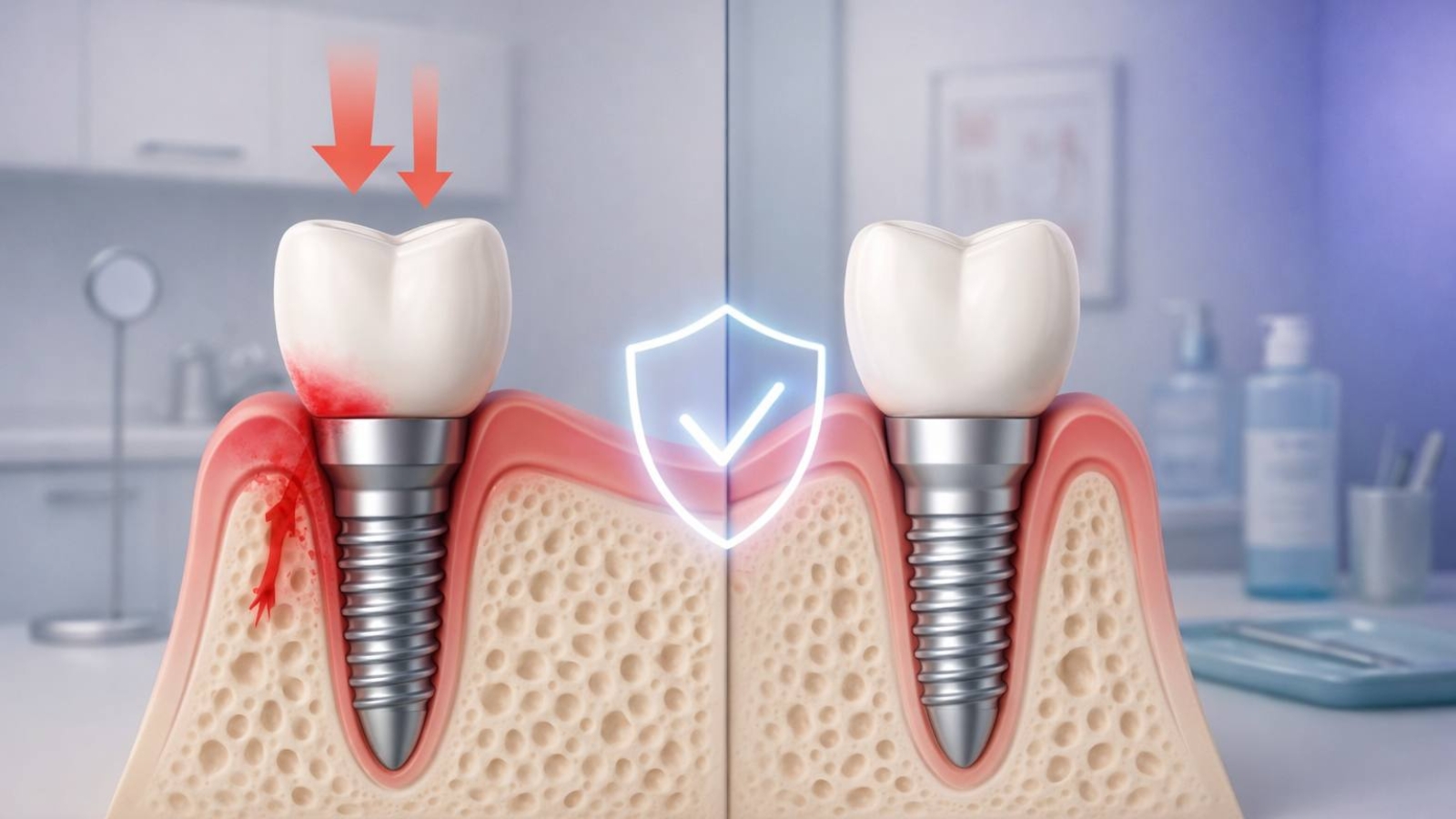
Unlike natural teeth, implants lack intrinsic adaptive capacity. They transmit load directly to the surrounding bone, meaning that any imbalance in force distribution can lead to overload. At DentalClinic24, clinicians evaluate not only bone volume and density, but also the direction of future masticatory forces, occlusal characteristics and the patient’s muscular activity patterns.
Occlusion is one of the most significant risk factors. Even minimal overloads in the implant zone-often imperceptible to the patient-can, over time, result in microdeformation of bone tissue or compromise the stability of the construction. At DentalClinic24, detailed occlusal analysis is used to identify potentially hazardous contact zones before prosthetic restoration is completed.
The number and positioning of implants are equally important. Attempting to compensate for an insufficient number of supports by increasing load on individual implants substantially raises the risk of complications. At DentalClinic24, treatment planning follows the principle of even force distribution rather than minimising implant numbers at any cost.
Muscular factors also influence long-term implant behaviour. Increased masticatory muscle tone, bruxism or asymmetrical jaw function can generate excessive loads that may not be apparent during routine examination. At DentalClinic24, overload risk assessment includes evaluation of neuromuscular coordination and functional mandibular movements.
Predicting implant performance is impossible without considering dynamics over time. What appears stable immediately after treatment may change as adaptive processes occur. At DentalClinic24, long-term prognosis accounts for potential changes in occlusion, muscle activity and bone condition.
When an increased risk of overload is identified, the treatment strategy is adjusted. This may involve modifying the prosthetic design, redistributing forces or revising the implantation scheme. Professor Alexander von Breuer notes that preventing overload is always more effective than treating its consequences.
For patients, this approach translates into greater reliability and predictability of results. When implants function within a biomechanically stable system, the risks of inflammation, bone loss and the need for repeat interventions are significantly reduced. At DentalClinic24, long-term stability is regarded as the primary criterion of successful implant therapy.
In conclusion, assessing the risk of implant overload is a critical stage of clinical planning. Analysis of occlusion, muscle activity and force distribution enables prediction of implant behaviour years into the future. At Dental Clinic24, this approach ensures not only functional success but also the longevity of implant-supported treatment.
Previously, we wrote about hidden disorders of chewing function at DentalClinic24 and why teeth may appear healthy while the system is already unstable