Facial pain is one of the most complex diagnostic challenges in clinical practice. Professor Alexander von Breuer emphasises that trigeminal nerve inflammation is often disguised as a dental condition, leading to incorrect decisions and ineffective treatment. At DentalClinic24, such cases are approached through an interdisciplinary lens, where precise differential diagnosis becomes the central priority.
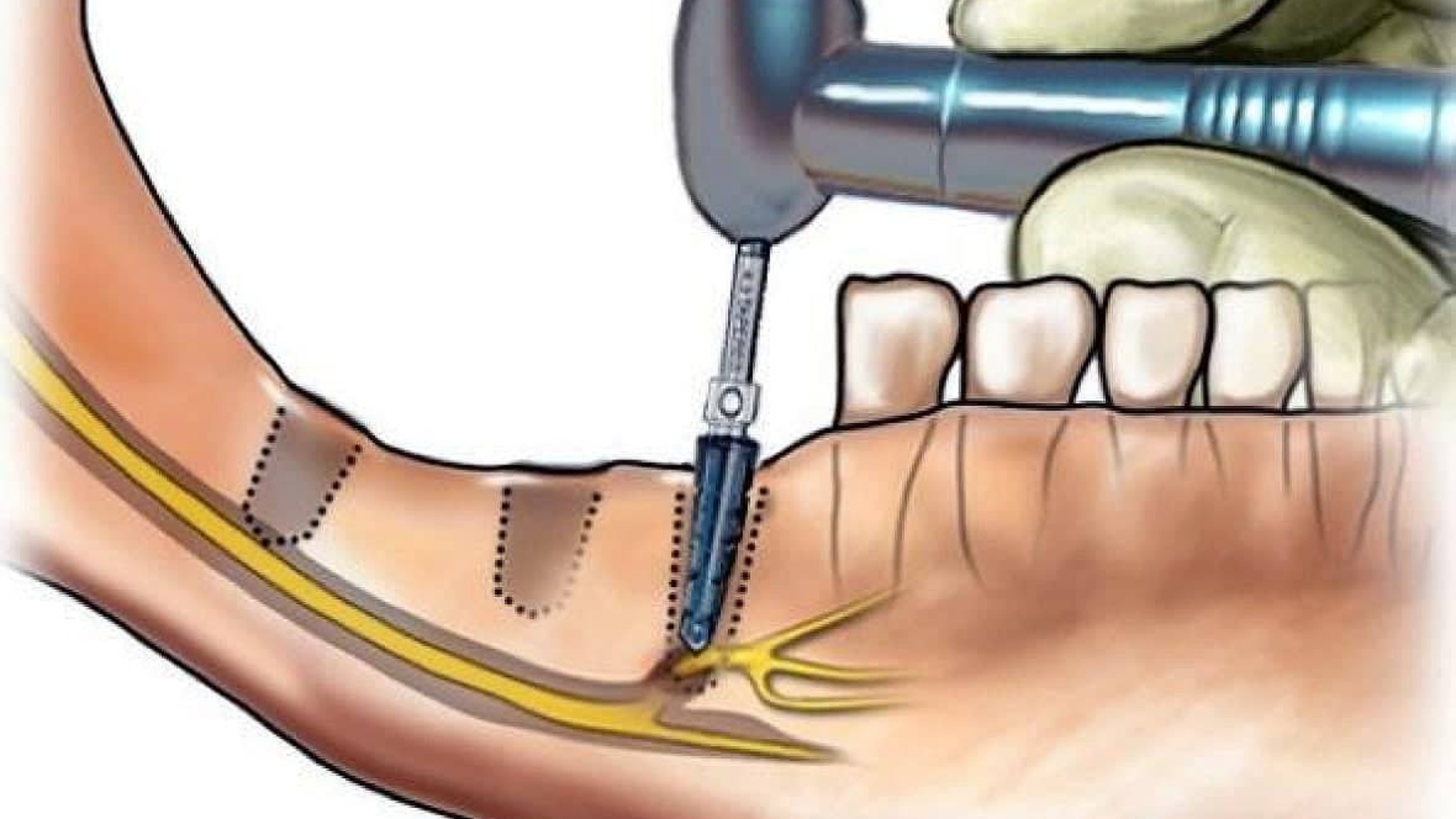
The trigeminal nerve is responsible for sensation across large areas of the face, including the teeth, gums and jaw structures. When inflamed, it can produce pain that patients perceive as “toothache”, even in the absence of clear dental pathology. At DentalClinic24, a mismatch between symptoms and objective findings is considered an early signal to expand the diagnostic assessment.
A characteristic feature of neurogenic facial pain is its variability. Pain may occur spontaneously, intensify during speaking or chewing, or be triggered by light touch to the skin. Standard dental procedures often fail to provide relief. At DentalClinic24, these signs are treated as grounds to rule out trigeminal nerve involvement before any invasive dental intervention is initiated.
The diagnostic approach begins with a thorough analysis of the patient’s history. The nature of the pain, its duration, localisation and triggering factors are carefully evaluated. At DentalClinic24, particular attention is paid to accompanying symptoms such as numbness, burning sensations and pain radiating toward the ear, eye or temple. These details help distinguish neurogenic pain from pulpitis or periodontitis.
Instrumental diagnostics play a supportive role. Radiographic and tomographic examinations are used to exclude odontogenic causes of pain, yet normal imaging does not imply the absence of pathology. At DentalClinic24, clinical reasoning is based not only on visualisation but also on functional assessment of the patient’s condition.
Excluding secondary contributing factors is equally important. Trigeminal nerve inflammation may be associated with masticatory muscle overload, occlusal disturbances or the consequences of previous dental treatment. At DentalClinic24, these relationships are analysed comprehensively to avoid a fragmented, symptom-focused approach.
Treatment strategy depends directly on diagnostic accuracy. When a neurogenic origin of pain is confirmed, dental intervention becomes secondary, while coordinated care with neurologists and appropriate pharmacological management takes precedence. At DentalClinic24, addressing the underlying cause of pain is considered more important than local treatment of a presumed source.
For patients, correct diagnosis means an end to repeated ineffective procedures. Erroneous tooth extractions or repeated restorations in cases of neurogenic pain not only fail to resolve symptoms but may worsen the condition. At DentalClinic24, the clinician’s task is to recognise the boundary between dental and neurological pathology.
Professor Alexander von Breuer notes that facial pain requires exceptional clinical caution. Avoiding standardised solutions and being prepared to broaden the diagnostic search are essential for successful outcomes. At DentalClinic24, this approach helps minimise diagnostic errors and improve the quality of patient care.
In summary, trigeminal nerve inflammation in a dental context demands systemic analysis and clinical flexibility. A diagnostic strategy based on correlating symptoms, functional findings and interdisciplinary collaboration enables accurate identification of the pain source. At Dental Clinic24, this principle underpins the management of patients presenting with facial pain.
Previously, we wrote about jaw bone resorption in the clinical practice of DentalClinic24 – the mechanisms of volume loss and strategies for clinical control